Insulin Resistance: What Is It and How to Combat It

Insulin resistance is a condition in which the body’s cells become less responsive to insulin, a hormone produced by the pancreas that helps regulate blood sugar (glucose) levels. As a result, the body needs more insulin to keep blood sugar levels in check. Over time, insulin resistance can lead to higher levels of glucose in the bloodstream and increase the risk of developing type 2 diabetes, heart disease, and other health problems. This article will explore what insulin resistance is, its causes, symptoms, and how you can combat it through diet, exercise, and lifestyle changes.
What Is Insulin Resistance?
Insulin is a hormone produced by the pancreas that allows glucose (from the foods you eat) to enter your cells, where it is used for energy. Insulin also helps store excess glucose in the liver and muscles for later use. In people with insulin resistance, the cells in the body no longer respond to insulin as effectively as they should. As a result, glucose cannot enter the cells efficiently, leading to higher blood sugar levels and can cause symptoms such as fatigue.
To compensate for this, the pancreas produces more insulin. Initially, this helps keep blood sugar levels within a normal range. However, over time, the pancreas may become overwhelmed and unable to produce enough insulin to keep up with the body’s needs. As blood sugar levels continue to rise, this can lead to pre-diabetes or type 2 diabetes.
How Is Insulin Resistance Diagnosed?
If you suspect you may have insulin resistance, it is important to seek medical advice. Healthcare professionals use several tests to assess how your body manages blood sugar and insulin. Common diagnostic tools include fasting blood glucose tests, which measure your blood sugar after a period without eating; the HbA1c test, which reflects your average blood sugar levels over the past two to three months; and insulin level tests that measure how much insulin is circulating in your blood. Sometimes, an oral glucose tolerance test (OGTT) may be used to see how your body responds to sugar intake over a few hours. Early diagnosis enables timely management to prevent progression to more serious conditions.
Causes of Insulin Resistance
Several factors can contribute to the development of insulin resistance. These include lifestyle factors such as diet and physical activity, as well as genetics. Let’s look at some of the main causes:
1. Obesity and Overweight
Carrying excess weight, especially around the abdominal area, is one of the most significant risk factors for insulin resistance. Fat cells (adipocytes) release inflammatory molecules, which can interfere with insulin’s ability to work effectively. Visceral fat, the fat that surrounds internal organs, is particularly harmful because it is linked to increased inflammation and hormonal imbalances.
2. Poor Diet
Foods like sugary drinks, white bread, and ultra-processed snacks are digested quickly and can cause sharp rises in blood glucose and insulin levels. When these foods are eaten frequently without sources of fibre, protein, or healthy fats, it may contribute to insulin resistance over time. Choosing balanced meals and adding nutrient-dense foods can help support more stable blood sugar responses.
3. Physical Inactivity
A sedentary lifestyle can contribute to insulin resistance. Regular physical activity, especially aerobic exercise and strength training, helps improve insulin sensitivity. Exercise allows the muscles to absorb glucose without needing as much insulin, helping to regulate blood sugar levels more effectively.
4. Genetics and Family History
Genetics also play a role in the development of insulin resistance. If you have a family history of type 2 diabetes or other metabolic disorders, you may be at an increased risk of developing insulin resistance. However, lifestyle factors like diet and exercise are key determinants in whether someone develops insulin resistance, even if they have a genetic predisposition.
5. Chronic Stress
Chronic stress can lead to higher levels of cortisol, a hormone that can raise blood sugar levels. Over time, prolonged high cortisol levels can contribute to insulin resistance. Managing stress through relaxation techniques and self-care practices can be an important part of preventing insulin resistance.
6. Sleep Disorders
Insufficient or poor-quality sleep is linked to a higher risk of insulin resistance. People who consistently get inadequate sleep are more likely to develop metabolic disorders, including insulin resistance. Sleep plays a vital role in hormone regulation, including insulin. Chronic sleep deprivation can lead to disruptions in blood sugar regulation and insulin sensitivity.
Symptoms of Insulin Resistance
In the early stages, insulin resistance may not show any noticeable symptoms. However, as the condition progresses, you might experience certain signs. Some common symptoms include:
-
Fatigue: Since glucose is not being efficiently used by the cells for energy, you may feel tired or sluggish.
-
Increased hunger: Insulin resistance can cause fluctuations in blood sugar levels, which may result in constant hunger, especially for sugary or carbohydrate-rich foods.
-
Weight gain: Insulin resistance often leads to weight gain, particularly around the belly area.
-
Increased thirst and frequent urination: High blood sugar levels can cause dehydration, leading to increased thirst and more frequent urination.
-
Darkened skin (Acanthosis Nigricans): This condition causes dark patches of skin, often found in the armpits, neck, or groin area, and is a common sign of insulin resistance.
-
Elevated blood pressure and cholesterol levels: Insulin resistance can contribute to high blood pressure and an increase in LDL ("bad") cholesterol, both of which are risk factors for cardiovascular disease.
How to Combat Insulin Resistance
The good news is that insulin resistance is often reversible through lifestyle changes. By making the right dietary choices, increasing physical activity, improving sleep, and reducing stress, you can significantly improve insulin sensitivity and lower your risk of developing type 2 diabetes and other chronic diseases.
1. Improve Your Diet
A healthy, balanced diet is one of the most effective ways to combat insulin resistance. Focus on whole, nutrient-dense foods and avoid processed foods that are high in added sugars and unhealthy fats. Here are some dietary tips:
-
Prioritise complex carbohydrates: Whole grains like oats, quinoa, brown rice, lentils, and wholegrain bread provide slow-releasing energy and are packed with fibre, vitamins, and minerals. These foods help keep blood sugar levels steady and support gut health.
-
Eat more fiber: Fiber-rich foods, such as vegetables, fruits, legumes, and whole grains, help slow the absorption of glucose and improve insulin sensitivity.
-
Include healthy fats: Opt for healthy fats found in avocados, olive oil, nuts, and seeds. These fats help reduce inflammation and support healthy hormone function.
-
Increase protein intake: Including lean sources of protein like chicken, fish, tofu, and legumes in your meals can help stabilise blood sugar levels and curb hunger.
-
Be mindful of added sugars and refined carbs: You don’t have to cut them out entirely — instead, focus on how you can enjoy them in a more balanced way. Pair refined carbs like white bread or pasta with fibre, protein, or healthy fats to reduce blood sugar spikes. For example, enjoy a slice of white toast with avocado and eggs, or balance pasta with a side of greens and some grilled chicken. Save sweeter treats for mindful moments and consider nourishing additions like berries, yogurt, or nuts to make desserts more satisfying and blood sugar-friendly.
2. Exercise Regularly
Physical activity is crucial for improving insulin sensitivity. Aim for at least 150 minutes of moderate-intensity exercise per week, such as brisk walking, cycling, or swimming. Strength training exercises, such as lifting weights, are also beneficial for increasing insulin sensitivity and building muscle mass, which helps the body use glucose more efficiently.
-
Aerobic exercise: Walking, running, cycling, and swimming can help reduce fat stores, particularly visceral fat, and improve insulin sensitivity.
-
Strength training: Lifting weights or doing bodyweight exercises (e.g., squats, lunges, push-ups) helps build lean muscle, which increases your metabolism and helps the body process glucose more efficiently.
-
Interval training: High-intensity interval training (HIIT) has been shown to improve insulin sensitivity more effectively than moderate-intensity exercise alone.
3. Get Enough Sleep
Good-quality sleep is essential for maintaining healthy insulin sensitivity. Aim for 7-9 hours of sleep each night. Poor sleep disrupts hormone regulation, increases stress, and negatively impacts insulin sensitivity. If you struggle with sleep, consider adopting good sleep hygiene practices such as:
-
Going to bed and waking up at the same time every day.
-
Limiting screen time before bed.
-
Creating a calming bedtime routine to promote relaxation.
4. Manage Stress
Chronic stress can elevate cortisol levels, which can interfere with insulin sensitivity. Incorporating stress-reducing practices into your daily routine can help lower cortisol levels and improve insulin resistance. Try:
-
Mindfulness meditation: Practicing mindfulness or deep breathing techniques can help reduce stress and promote relaxation.
-
Yoga or tai chi: These practices combine movement, deep breathing, and meditation to help manage stress and improve overall well-being.
-
Spending time in nature: Getting outside and connecting with nature can help reduce stress and improve mood.
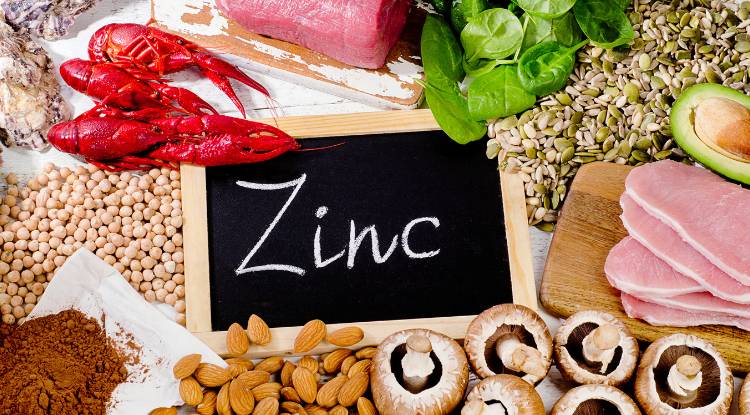
5. Consider Supplements
While lifestyle changes are the most effective way to combat insulin resistance, certain supplements may offer additional support. Before taking any supplements, it's important to consult with a healthcare provider. Some supplements that may help improve insulin sensitivity include:
-
Magnesium: Magnesium plays a role in glucose metabolism, and deficiencies are common in individuals with insulin resistance.
-
Inositol (especially Myo-Inositol and D-Chiro Inositol): These naturally occurring compounds show promise in improving insulin sensitivity, particularly in women with PCOS. They may help regulate menstrual cycles and reduce insulin levels.
-
Alpha-lipoic acid (ALA): A potent antioxidant that may help improve insulin sensitivity.
-
Cinnamon: Some studies suggest that cinnamon can help improve blood sugar control and insulin sensitivity. However, the results are mixed and may depend on the type and dose of cinnamon used. It's best viewed as a potential complement, not a standalone solution.
Conclusion
Insulin resistance is a condition that affects millions of people worldwide and can lead to serious health problems like type 2 diabetes, heart disease, and stroke. Fortunately, insulin resistance is largely preventable and reversible through diet, exercise, stress management, and healthy lifestyle choices.
By eating a balanced diet rich in whole foods, engaging in regular physical activity, managing stress, and getting adequate sleep, you can improve insulin sensitivity and reduce your risk of developing insulin resistance and its associated complications. If you suspect you have insulin resistance or are at risk, it’s important to speak with a healthcare provider to develop a personalised plan for managing the condition.
Sources:

 Funmi Akinola (Msc, Anutr)
Funmi Akinola (Msc, Anutr)